
When it comes to treating certain gynecological conditions like fibroids, adenomyosis, abnormal uterine bleeding not responding to conservative treatment, hysterectomy remains a common surgical intervention. However, there are different approaches to this procedure, each with its own benefits and considerations. In this blog post, we will delve into the key distinctions between total hysterectomy and supracervical hysterectomy, highlighting their pros and cons to help you make a more informed decision.
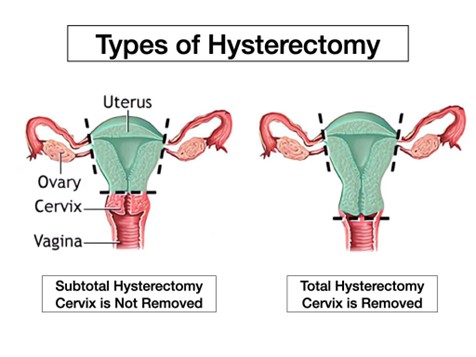
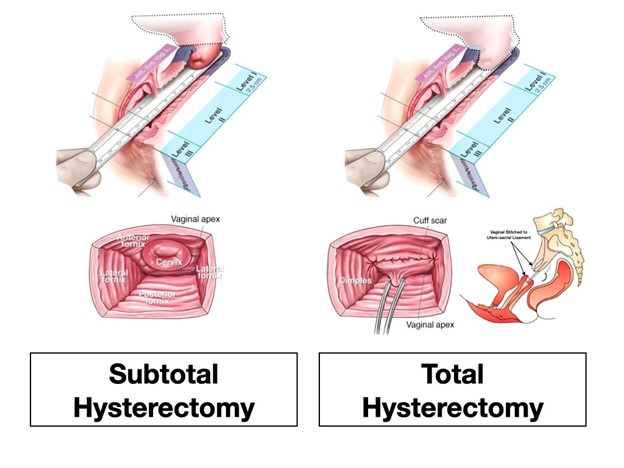
A total hysterectomy involves the removal of both the uterus and the cervix. It is often the preferred choice for certain conditions, such as cancerous or precancerous conditions, extensive endometriosis, multiple fibroids and cases involving abnormal bleeding.
Elimination of Gynecological Conditions: By removing both the uterus and cervix, a total hysterectomy can effectively eliminate conditions such as uterine fibroids, endometriosis, adenomyosis, and certain types of cancer.
Reduced Risk of Recurrence: With the removal of both the uterus and cervix, there is a reduced risk of recurrent conditions in those cases where the cervix may contribute to the recurrence of certain diseases.
Enhanced Diagnostic Accuracy: Removing the entire uterus allows for a more accurate examination of the uterine tissue, which can help in identifying and treating potential abnormalities.
Recovery Time: Total hysterectomy may require a slightly longer recovery period compared to supracervical hysterectomy due to the nature of the procedure.
Impact on Sexual Function: In total hysterectomy, it is generally recommended to abstain from intercourse for 10-12 weeks, whereas in supracervical hysterectomy, resumption of sexual activity can occur in 4 weeks. Removal of the cervix during total hysterectomy may affect sexual sensation, although individual experiences may vary.
Supracervical hysterectomy, also known as partial hysterectomy, involves removing the uterus while preserving the cervix. This technique has gained popularity in recent years due to its potential advantages in terms of quicker recovery and better sexual function.
Preserved Cervix: By keeping the cervix intact, supracervical hysterectomy may preserve the natural support of the upper vagina, potentially minimizing post-surgical changes to sexual function.
Shorter Recovery Time: The less invasive nature of supracervical hysterectomy often results in a shorter recovery period, allowing patients to return to their daily activities more quickly.
Lower Risk of Surgical Complications: With fewer structures being removed, there is generally a reduced risk of complications such as bladder or bowel injury during the procedure, though it doesn’t make much difference in experienced hands.
Continued Cervical Cancer Screening: Since the cervix is retained, regular cervical cancer screenings, including Pap smears, are still necessary to monitor any potential abnormalities.
Potential for Cervical-Related Conditions: Although the cervix is preserved, there is still a possibility of developing cervical-related conditions such as cervical dysplasia, cervical polyps, cervical fibroid, or cervical cancer in the future.
Potential for Residual Menstrual Symptoms: While the uterus is removed, some women may experience residual symptoms like cyclical bleeding or menstrual-like pain due to hormonal fluctuations, persistence of pelvic pain to some extent in severe pelvic endometriosis.
The Journal of Sexual Medicine, 2023, 20, 447–466
Hysterectomy and sexual function: a systematic review and meta-analysis:
Conclusion: Subtotal and total hysterectomy was not associated with significant change in overall sexual function irrespective of surgical route
The American Journal of Obstetrics and Gynecology, Volume 212, Issue 6, June 2015, Pages 758.e1-758.e54
Subtotal versus total abdominal hysterectomy: randomized clinical trial with 14-year questionnaire follow-up
Conclusion: Subtotal abdominal hysterectomy was not superior to total abdominal hysterectomy on any outcomes. More women seem to have subjective urinary incontinence 14 years after subtotal abdominal hysterectomy.
The Journal of Sexual Medicine, Volume 3, Issue 3, May 2006, Pages 483–491
The Psychosocial Outcomes of Total and Subtotal Hysterectomy: A Randomized Controlled Trial
Conclusions: Hysterectomy resulted in a consistent reduction in abdominal pain, some improvement in sexual functioning, but no change in overall psychological functioning. There was no evidence supporting the idea that subtotal hysterectomy produced more favorable psychosocial outcomes than total hysterectomy nor was there any evidence that either type of hysterectomy resulted in adverse effects.
Total or Supracervical Hysterectomy Research Group, Obstet Gynecol. 2003;102:453–462.7 Level I evidence
A randomized comparison of total or supracervical hysterectomy: Surgical complications and clinical outcomes.
Conclusions: We found no statistically significant differences between supracervical hysterectomy and total abdominal hysterectomy in surgical complications and clinical outcomes during 2 years of follow-up.
OBG Manag. 2004 September;16(9):32-45
Subtotal vs total hysterectomy: Does the evidence support saving the cervix?
KEY POINTS
Sexual function is not improved more with supracervical than with total hysterectomy.
Operative morbidity for supracervical and total hysterectomy are similar.
Pelvic-floor support and urinary incontinence do not seem to be improved with the supracervical approach.
Cyclic bleeding occurs in 5% to 20% of women after supracervical hysterectomy.
Reoperation rates for symptoms related to the retained cervix are significant—over 20% in the hands of highly skilled surgeons.
Total hysterectomy and supracervical hysterectomy are two distinct surgical approaches, each with their own advantages and considerations. The choice between the two depends on several factors, such as the patient's medical condition, age, previous surgeries, and personal preferences.
Based on the available literature and medical evidence, we conclude that supracervical hysterectomy is an alternative to total laparoscopic hysterectomy, offering a lower incidence of bladder injury, particularly in cases with previous cesarean sections. It also allows for earlier resumption of sexual activity. However, cervical preservation carries a small risk of bleeding, pelvic pain, and malignant transformation, which may require further intervention.
On the other hand, total laparoscopic hysterectomy has a lower incidence of reoperation and eliminates complications associated with the cervical stump. However, it is associated with an increased risk of urinary tract injury, particularly in the hands of inexperienced surgeons. The decision to perform either procedure depends on the surgeon's expertise and the preferences of both the surgeon and the patient.
It is crucial to have a thorough discussion with your healthcare provider to evaluate the most appropriate option for your specific circumstances. Remember, making an informed decision is essential for your overall well-being and future health.
MBBS, MD(Obs&Gn), FMIS(Laparoscopy)
Head of the Department Obstetrics & Gynecology
Advanced Gynecological Laparoscopic Surgeon
& Pelvic Reconstructive Surgeon
MEDICLINIC WELCARE HOSPITAL
Al Garhoud, Dubai
MEDICLINIC PARKVIEW HOSPITAL
Umm Sequim, Al Barsha South 3, Dubai
Appointments 800-1999
www.mediclinic.ae
