Hysterectomy is a common gynecological procedure which involves removal of uterus. It does not necessarily mean removal of the ovaries. As the main functions of the uterus are reproduction and menstruation, a hysterectomy would therefore mean you no longer can bear children nor have menstruation.
When is a Hysterectomy advised in fibroid?
Uterus removal or hysterectomy is advised in a woman with fibroid when she is not finding relief of her symptoms with medical management or with uterine conservative procedures like uterine artery embolization or myomectomy. Hysterectomy is advised as a primary treatment in symptomatic women with multiple large fibroids who is not wishing to have children or completed fertilityfunction.
What are the different methods of doing hysterectomy?
The three main methods of hysterectomy are:
Vaginal Hysterectomy
The vaginal route is suitable where the uterus is prolapsed and is not too large. The entire hysterectomy is performed through the vaginal route.
Abdominal Hysterectomy
The abdominal route remains the common method of hysterectomy. But it is not the ideal method due the bigger cut in the abdomen, more pain and longer stay in hospital compared to laparoscopic hysterectomy.
Laparoscopic Hysterectomy
The laparoscopic route is a minimally invasive surgical procedure to remove the uterus. It is performed through three to four small skin incisions, is a safe and effective alternative method to abdominal surgery when performed in the hands of surgeons trained in laparoscopic surgery.
The route of surgery is often determined by the indication for hysterectomy, the severity of the pathology, and the surgical skills and experience of the surgeon. While it is natural for most women to go for the least invasive method, ultimately, you should discuss with your doctor who will advise and choose the safest route for your hysterectomy.
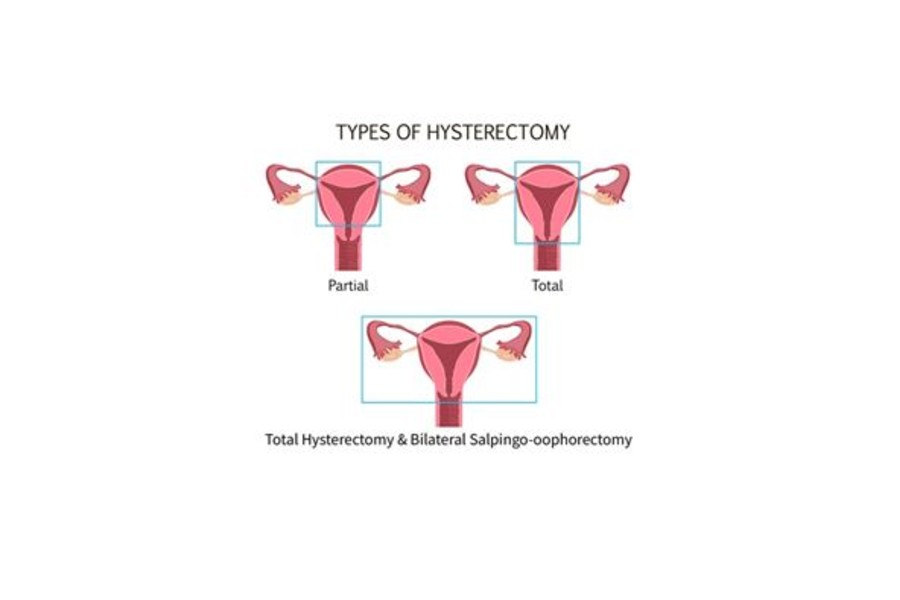
Different types of Laparoscopic hysterectomy
Total Laparoscopic hysterectomy – Removal of the uterus and cervix. The ovaries are preserved. In pre-menopausal women, this means there is no change in hormonal status.
Laparoscopic Subtotal hysterectomy – The cervix of the uterus is preserved. Routine cervical screening is necessary.
Total Laparoscopic hysterectomy – Removal of the uterus and cervix. The ovaries are preserved. In pre-menopausal women, this means there is no change in hormonal status.
Total Laparoscopic hysterectomy and bilateral-salpingooophorectomy – Removal of the uterus, cervix, ovaries and fallopian tubes – in pre-menopausal women this would mean a loss of ovarian hormones. In turn, this means you will go into menopause. In postmenopausal women, there is no hormonal change as the ovaries have already stopped functioning.
Why is Laparoscopic Hysterectomy preferred over open abdominal hysterectomy?
The advantages of laparoscopic hysterectomy compared to abdominal hysterectomy have been well documented. The advantages have been firmly established to include reduced short-term morbidity like
Less pain
Less blood loss
Less scarring and wound Infection
Faster recovery
Shorter hospital stays
Earlier return to work and normal activity
Whether laparoscopic hysterectomy can be done in all cases like large uterus, in patients with previous multiple surgeries?
Laparoscopic Hysterectomy in patients with Previous Cesarean Section
Total laparoscopic hysterectomy (TLH) in the presence of patients with previous cesarean section (CS) is becoming increasingly common. When performing TLH in these patients, bladder adhesions to the uterus may make dissection much more difficult with increased risk of Urinary Bladder injury.
But Laparoscopic hysterectomy in patients with 1 or more previous CS is technically feasible in the hands of thoroughly trained laparoscopic surgeons using a standardized technique. It is a safe procedure with minimal complication rates irrespective of the size of the uterus or the number of previous cesarean sections.
Is Laparoscopic hysterectomy safe in morbidly obese patients?
Morbidly obese patients are a vulnerable group of patients; they have a lot of medical co morbidities, and when they need surgery, they have an increased risk of having poor perioperative outcomes because of their BMI.
Compared to both laparoscopic and VH, the abdominal approach in patients with a BMI ≥35 kg/m2 is associated with more postoperative complications and longer length of hospital stay. Compared to open abdominal hysterectomy, both the laparoscopic and vaginal approaches are associated with a significantly lower incidence of postoperative complications. With Laparoscopic Hysterectomy there is a lower risk of wound infection, Dehiscence, Incisional hernia formation and reduced risk of Deep Vein thrombosis due to early ambulation in laparoscopic procedures
What are the side-effects of hysterectomy?
Women are often anxious about a range of side-effects when considering hysterectomy. The common concerns are emotional, hormonal and sexual side-effects.
Emotional effects – The emotional effects of hysterectomy vary from person to person and may be expected or unexpected. Some women feel sad and depressed about the loss of reproduction, while others feel relieved as contraception is no longer required. Some women are delighted with the marked improvement in their well-being as hysterectomy brings to an end of years of chronic pain and heavy bleeding. By talking about your feelings freely with your partner or your doctor before and after the operation, you will often find a great deal of support to help you get through the difficult times.
Hormonal effects – In general, if you are premenopausal at the time of hysterectomy and choose to keep the ovaries, you should not experience any sudden hormonal change. If the ovaries are removed, then you can expect the menopausal effects soon after the operation, with symptoms such as hot flushes, insomnia, lethargy and mood fluctuations. In this case, discuss with your doctor about HRT or alternative options. On the other hand, you should notice no difference if the ovaries are removed after your natural menopause.
Sexual effects – A hysterectomy will put your sex life on pause for a few weeks, but it shouldn’t end it. The effect of hysterectomy on sexuality remains unclear with conflicting evidence from research. This is probably because sexuality is not only personal and hence is often difficult to study and measure. According to studies most women said their sex life either stayed the same or improved after the procedure. They were finally free from the pain or heavy bleeding that caused them to have the surgery.
But Hysterectomy with removal Ovaries Can reduce your desire for sex. That’s because your ovaries produce testosterone and estrogen — hormones that are integral to your libido.
How long does the surgery take?
On average, the duration of Laparoscopic Hysterectomy takes around 30 – 120 minutes. The duration of surgery depends on the size of uterus, presence of adhesions and the experience of surgeon.
What can I expect after a laparoscopic hysterectomy?
Usual length of stay in hospital
In most instances, you will be admitted to hospital on the day of your operation. You may be able to go home after24 hours or, depending on your circumstances, you may need to stay in hospital for one to three days.
After-effects of general anesthesia
Most modern anesthetics are short lasting. You should not have, or suffer from, any after-effects for more than a day after your operation. During the first 12 hours you may feel more sleepy than usual. You are likely to be in hospital during the first 24 hours but, if not, you should have an adult with you during this time and you should not drive or make any important decisions.
Catheter
Generally, after laparoscopic hysterectomy no urinary catheter is placed, and you are allowed to walk to the toilet to empty your bladder. You may have a catheter (tube) in your bladder to allow drainage of your urine in certain cases where the urinary bladder is densely adherent to uterus as in case of previous cesarean sections. This is usually for up to 24 hours after your operation. If you have problems passing urine, you may need to have a catheter for a few days.

Scars
You will have between three or four small scars on different parts of your abdomen of 0.5cm to 1 cm. If you have had your cervix removed, you will stitch at the top of your vagina.
Stitches and dressings
Cuts on your abdomen will be closed by stitches or glue. Glue and stitches dissolve by themselves. Your cuts will initially be covered with a dressing. You should be able to take this off about 24 hours after your operation and have a wash or shower.
Any stitches in your vagina will not need to be removed, as they are dissolvable. You may notice a stitch, or part of a stitch, coming away after a few days or maybe after a few weeks. This is normal and nothing to worry about.
Vaginal bleeding
You can expect to have some vaginal bleeding for one to three weeks after your operation. This is like a light period and is red or brown in color. Some women can have sudden gush of blood about 14-28 days later. If the bleeding is not stopping and heavy bleeding continues then it’s a sign of secondary hemorrhage and you need to consult your doctor immediately which requires immediate attention. You should use sanitary towels rather than tampons as using tampons could increase the risk of infection.
Pain and discomfort
You can expect pain and discomfort in your lower abdomen for at least the first few days after your operation. Some patients may experience pain in shoulder, this is common after laparoscopic surgery and usually subsides in 24-36 hours. When leaving hospital, you will be provided with painkillers for the pain you are experiencing. Sometimes painkillers that contain codeine or dihydrocodeine can make you sleepy and constipated. If you do need to take these medications, try to eat extra fruit and fiber to reduce the chances of becoming constipated. Taking painkillers as prescribed to reduce your pain will enable you to get out of bed sooner and move around – all of which will speed up your recovery and help to prevent the formation of blood clots in your legs or your lungs.
Starting to eat and drink
After your operation, you may have a drip in your arm to provide you with fluids. You will be started with oral fluid after 4- 6 hours of surgery. When you are able to drink and eat comfortably, the drip will be removed. You will be offered a drink of water or cup of tea and something light to eat. Following operation your bowel may temporarily slow down, causing air or ‘wind’ to be trapped. This can cause some pain or discomfort until it is passed. Getting out of bed and walking around will help. Mostly within 24 hours you will be allowed to have a regular diet.
Washing and showering
You should be able to have a shower or bath and remove any dressings the day after your operation. Don’t worry about getting your scars wet – just ensure that you pat them dry with clean disposable tissues or let them dry in the air. Keeping scars clean and dry helps healing.

When should I seek medical advice after a laparoscopic hysterectomy?
While most women recover well after a laparoscopic hysterectomy, complications can occur – as with any operation.
Burning and stinging when you pass urine or pass urine frequently: This may be due to a urine infection. Treatment is with a course of antibiotics.
Vaginal bleeding that becomes heavy or smelly: If you are also feeling unwell and have a temperature (fever), this may be due to an infection or a small collection of blood at the top of the vagina called a vault hematoma. Treatment is usually with a course of antibiotics. Occasionally, you may need to be admitted to hospital for the antibiotics to be administered intravenously (into a vein). Rarely, this blood may need to be drained.
Red and painful skin around your scars: This may be due to a wound infection. Treatment is with a course of antibiotics.
Increasing abdominal pain: If you also have a temperature (fever), have lost your appetite and are vomiting, this may be due to damage to your bowel or bladder, in which case you will need to be admitted to hospital.
A painful, red, swollen, hot leg or difficulty bearing weight on your legs: This may be due to a deep vein thrombosis (DVT). If you have shortness of breath or chest pain or cough up blood, it could be a sign that a blood clot has travelled to the lungs (pulmonary embolism). If you have these symptoms, you should seek medical help immediately.
Getting back to normal
Exercise: While everyone will recover at a different rate, there is no reason why you should not start walking on the day you return home. You should be able to increase your activity levels quite rapidly over the first few weeks. There is no evidence that normal physical activity levels are in any way harmful and a regular and gradual buildup of activity will assist your recovery. If you are unsure, start with short steady walks close to your home a couple of times a day for the first few days. When this is comfortable, you can gradually increase the time while walking at a relaxed steady pace. Many women should be able to walk for 30- 60 minutes after two or three weeks. If you build up gradually, most women should be back to previous activity levels within four to six weeks.
Having sex: You should usually allow eight – ten weeks after your operation to allow your scars to heal. It is then safe to have sex – if you feel comfortable. If you experience any discomfort or dryness (which is more common if your ovaries have been removed at the time of the hysterectomy), you may wish to try a vaginal lubricant. You can buy this from your local pharmacy.

Driving: Before you drive you should be:
• Free from the sedative effects of any painkillers
• Able to sit in the car comfortably and work the controls
• Able to wear the seatbelt comfortably
• Able to make an emergency stop
What to expect on follow up Visits?
Starting HRT (hormone replacement therapy)
If your ovaries have been removed during your operation, you may be offered hormone replacement therapy (HRT). This will be discussed with you by your gynecologist and together you can decide the best way forward.
A pelvic floor muscle exercise
Your pelvic floor muscles span the base of your pelvis. They work to keep your pelvic organs in the correct position (prevent prolapse), tightly close your bladder and bowel (stop urinary or anal incontinence) and improve sexual satisfaction. It is important for you to get these muscles working properly after your operation, even if you have stitches. To identify your pelvic floor muscles, imagine you are trying to stop yourself from passing wind, or you could think of yourself squeezing tightly inside your vagina. When you do this, you should feel your muscles ‘lift and squeeze’. It is important to breathe normally while you are doing pelvic floor muscle exercises. You may also feel some gentle tightening in your lower abdominal muscles. This is normal.






